Governor Greg Abbott issued a statewide disaster declaration Thursday, January 29th to prevent a certain species of screwworm fly from entering Texas, mobilizing state resources against a parasite. “Although… not yet present in Texas or the U.S., its northward spread from Mexico toward the U.S. southern border poses a serious threat,” Abbott stated.
Cochliomyia hominivorax, also called Coquerel or New World screwworms, are parasites endemic in South America and the Caribbean. Not new to America, the U.S. was declared free of the parasite in 1966 by the US Department of Agriculture, after successful eradication efforts. A small outbreak occurred in the Florida Keys in 2017.

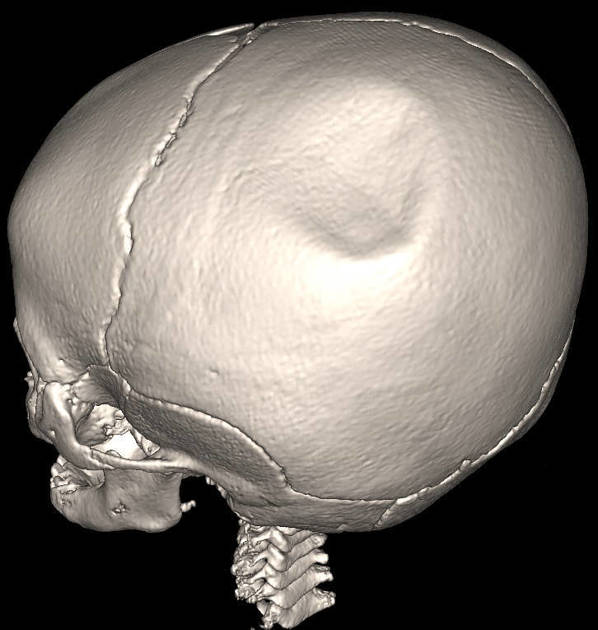
According to the US Embassy in Costa Rica, “screwworm flies predominantly affect cattle, but frequently affect dogs… and occasionally affect humans.” Experts warn that maggots can burrow into vulnerable tissue like the brain, causing sepsis. Sepsis can cause severe brain damage through systemic inflammation, disrupting the blood-brain barrier (BBB), oxygen deprivation, and neuroinflammation, leading to acute issues like delirium and coma, and long-term cognitive deficits. The Embassy further discusses the story of a 15-year-old girl developed intense headaches after 45 larvae infested a scalp wound, demonstrating risks to children and representing the first human death since the 1990s.
Protection requires cleaning and covering all wounds, wearing long-sleeved clothing, and using EPA-registered insect repellents.