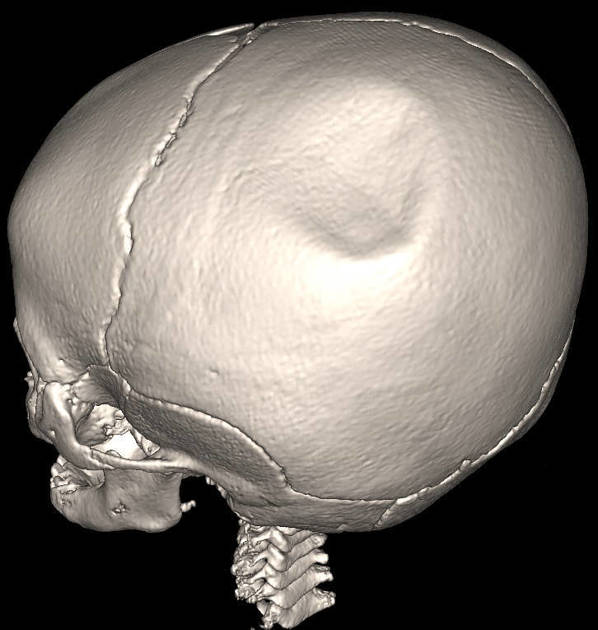
This Valentine’s Day, that box of dark chocolates may offer more than romance. A body of research indexed in PubMed reveals that dark chocolate’s primary flavanol, epicatechin, is a potent neuroprotective compound with remarkable potential for brain injury recovery.
“Epicatechin represents a promising therapeutic candidate for traumatic brain injury – its multi-pathway neuroprotection, from antioxidant defense to neurogenesis, makes it unlike any single pharmaceutical agent,” stated Wang et al. in 2024 in CNS Neuroscience & Therapeutics. Research shows that administering epicatechin after traumatic brain injury prevents neuronal death, reduced neuroinflammation, and restored neurological function by targeting the AKT-P53/CREB signaling pathway. This pathway then promotes cell growth and inhibits apoptosis. A 2025 meta-analysis in the Journal of Agricultural and Food Chemistry pooled 12 animal studies and confirmed epicatechin significantly improves outcomes across TBI, ischemic stroke, and other brain injury types, while reducing oxidative stress and boosting antioxidant defenses.
Dark chocolate’s brain benefits operate through multiple pathways: boosting cerebral blood flow by 8-10% via nitric oxide–mediated vasodilation, activating the Nrf2 antioxidant system, elevating the brain-derived neurotrophic factor critical for neuronal survival, and stimulating neurogenesis. Crucially, these are the very mechanisms disrupted by traumatic brain injury and stroke.
While most current TBI-specific evidence remains in animal models, the results are compelling. This Valentine’s Day, choose dark chocolate with the highest cocoa content you can find, preferably 70% or above. Your brain, and your loved one’s brain, will thank you.