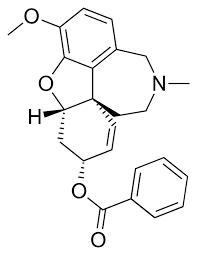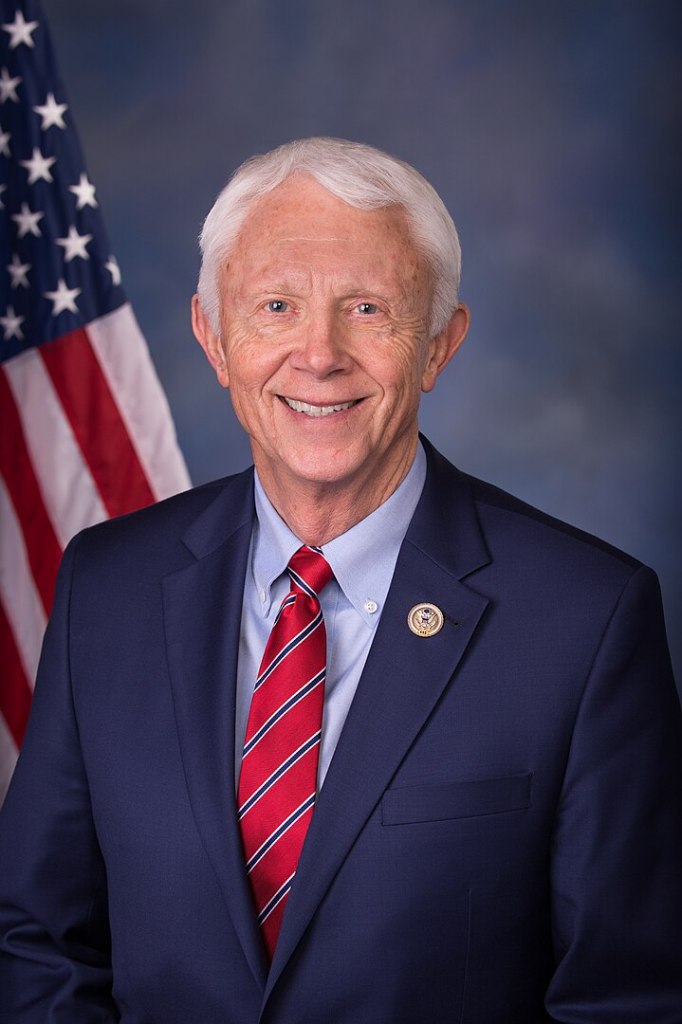
Representative Jack Bergman (MI), along with 5 original co-sponsors [Sarah Elfreth (MD), Kimberlyn King-Hinds (MP), Donald G. Davis (NC), Derrick Van Orden (WI), Morgan Luttrell (TX)] introduced the BEACON Act, H. R. 6993, in January 2026 to transform how the Department of Veterans Affairs treats traumatic brain injuries. The Veterans TBI Breakthrough Exploration of Adaptive Care Opportunities Nationwide Act establishes two grant programs totaling $60 million to fund innovative, non-pharmacological treatments for mild-to-moderate TBI.*

The sponsor of the bill and at least one of its co-sponsors bring personal stakes to this fight. Bergman, a retired Marine Lieutenant General with 40 years of service including Vietnam combat, witnessed how invisible injuries affect service members. Elfreth watched her grandfather – a Korean and Vietnam War veteran – suffer from PTSD, inspiring her earlier success passing Maryland’s David Perez Military Heroes Act.
Veterans often feel “unseen, unheard, and alone” navigating systems that treat symptoms rather than people. The BEACON Act addresses these gaps by funding research into evidence-based alternatives, training clinicians, and partnering academic institutions with VA facilities to bring innovative care directly to veterans.
*Per bill text, the TBI Innovation Grant Program will “award grants to eligible entities… for the development, implementation, and evaluation of approaches and methodologies for prospective randomized control trials for 11 neurorehabilitation treatments for the treatment of chronic mild TBI (mTBI) in veterans.” Additionally, the Act with provide grants for “independent third-party research studies and treatment with respect to supplemental neurorehabilitation treatments of mTBI.”