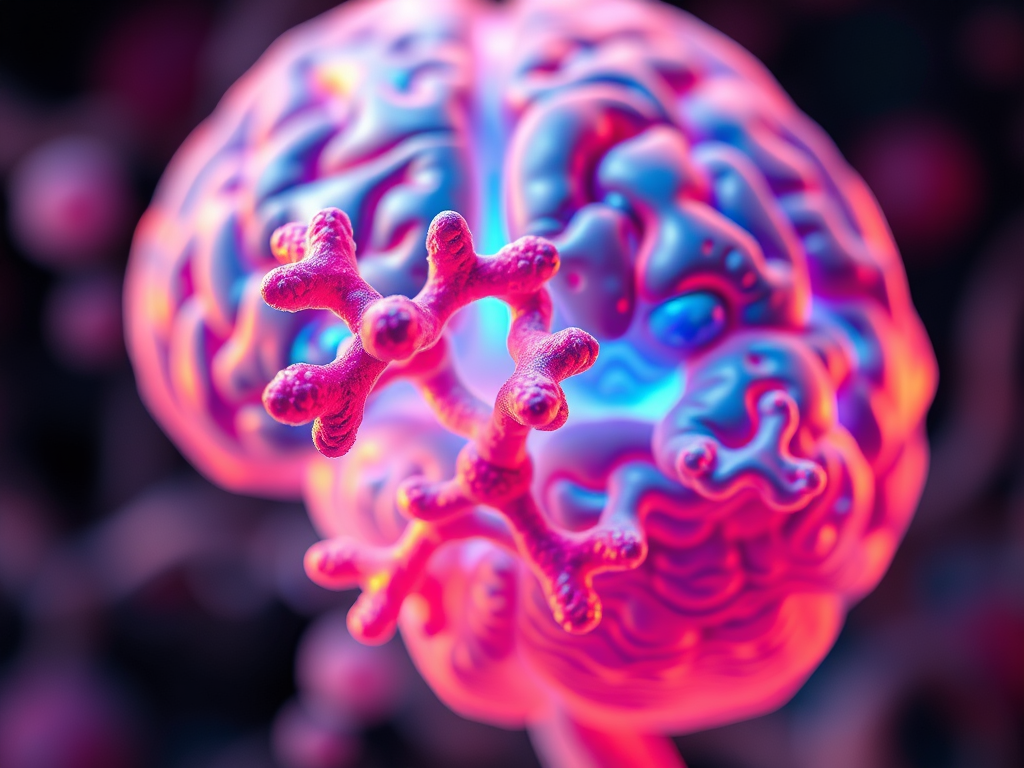
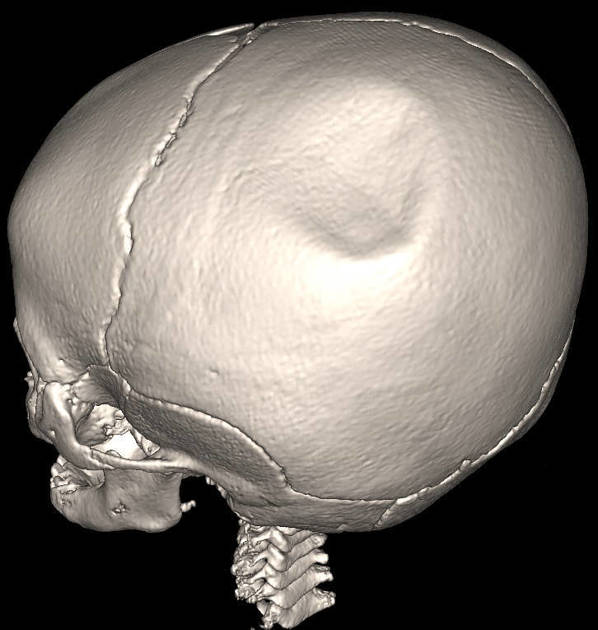
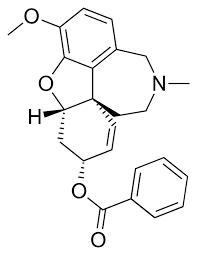
On January 23, 2026, the Journal of Neurotrauma reported on a form of preventative treatment for CTE, and other forms of brain injury: near-infrared light therapy. According to the article, this form of therapy, also known as photobiomodulation, “shines powerful near-infrared light at the brain through the skull, may be able to prevent or reduce subtle damage to the brain before symptoms start, by reducing brain inflammation caused by repetitive impacts.”
While infrared light therapy may be lesser-known, reports show that the red light therapy and its benefits have, in fact, been known and ongoing for over a decade. Studies indicate this non-invasive, home-based therapy improves cognition, reduces PTSD symptoms, and increases cerebral blood flow by stimulating mitochondrial functio.
Athletes who received this infrared light show significant reductions in markers of neuroinflammation and axonal stress compared to their pre-season baseline, suggesting the therapy preserves neural integrity. Dr. Carrie Esopenko, associate professor of neurology at University of Utah that, along with NYU, is running a four-year government-funded study on the treatment, hopes “the results will help keep athletes healthy across all sports” while ensuring families “can participate in sports safely for the long term.” Boston University Medical Campus is also investigating transcranial photobiomodulation (tPBM) using red and near-infrared LED devices to treat chronic traumatic brain injury (TBI) and PTSD.