During severe weather at Utah’s RedWest music festival in October 2025, a 2’x12’ scaffolding board broke loose from a nearby construction site and struck 23-year-old Ava Ahlander, killing her instantly. This tragedy underscores construction scaffolding’s critical vulnerability—despite providing essential support for workers, these temporary structures can traumatically injure or turn deadly when they fail.
The stakes are staggering. “In 2023, 5,283 workers lost their lives. That means a worker dies every 99 minutes,” stated Assistant Secretary of Labor for Occupational Safety and Health Doug Parker in December 2024. While that death rate is a conglomeration of all construction deaths, in 2022 alone, falls from elevation claimed 365 construction workers’ lives – additionally, it does not note the rate of disability.
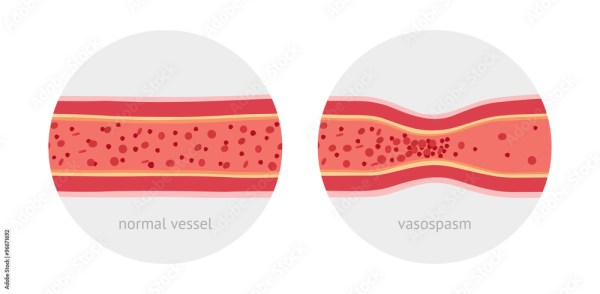
Yet inside our skulls exists another type of scaffolding—neural networks that support brain function. Unlike construction platforms that can be dismantled and rebuilt, brain scaffolding faces unique repair challenges. Traumatic brain injury severely limits the brain’s natural regeneration capacity.
Now researchers are developing biodegradable polymer scaffolds seeded with neural progenitor cells to bridge the gap. These biological structures can reduce lesion volume, promote neurite outgrowth, and significantly improve motor function after brain injury. As noted in a June 2025 NIH-published study How neural stem cell therapy promotes brain repair after stroke, understanding how these stem cell grafts promote neural repair “remains incompletely understood.”
While construction scaffolding must be secured to prevent tragedy, our own scaffolding benefits from neuroplasticity—the remarkable ability to reorganize and heal.