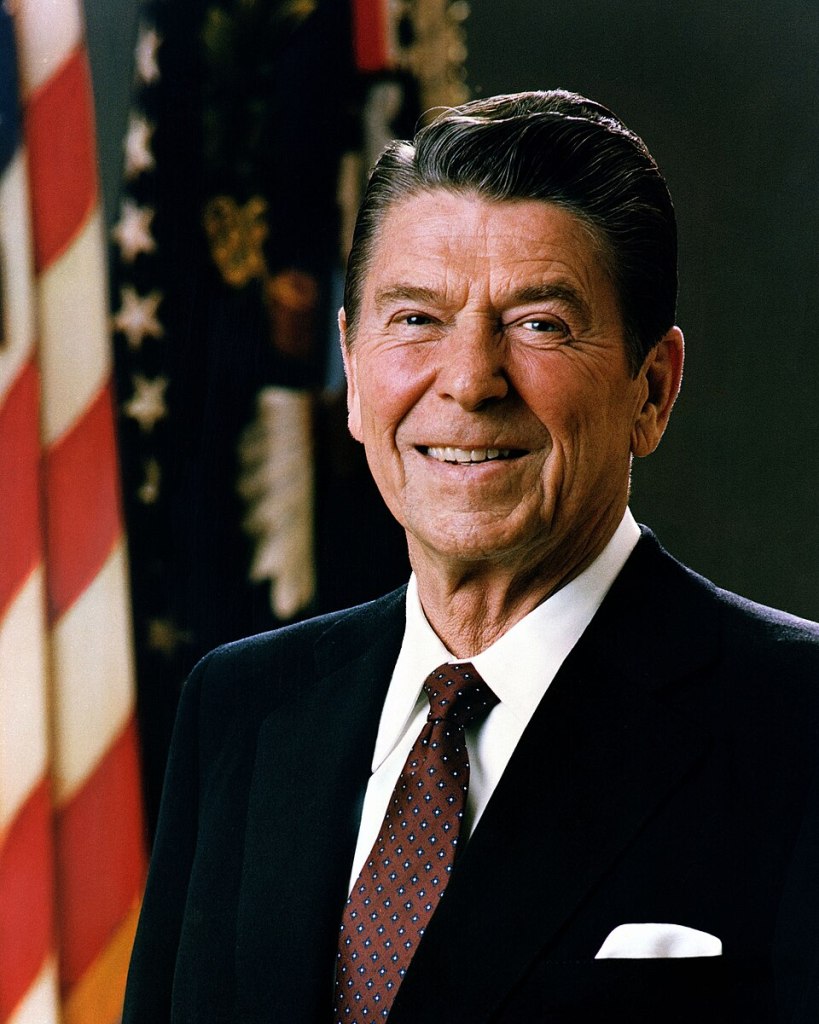
On what would have been his 115th birthday, TBIontheHill honors Ronald Reagan, America’s 40th President of the United States:
President Ronald Reagan left an enduring mark on the brain injury community when he signed Proclamation 5262 in October 1984, designating National Head Injury Awareness Month. This landmark action acknowledged the 700,000 Americans hospitalized annually for head injuries and called for greater research and support.
Reagan himself experienced traumatic brain injury firsthand. On July 4, 1989 – just months after leaving office – the 78-year-old was thrown from a bucking horse at a friend’s ranch in Mexico. The fall caused a subdural hematoma, a dangerous blood clot between the brain and skull. After initial treatment, doctors discovered a second clot requiring brain surgery at the Mayo Clinic in September 1989.
Because the accident occurred after his presidency, it did not affect his time in office. However, Nancy Reagan later wrote that she believed the severe head injury “hastened the onset” of her husband’s Alzheimer’s disease, diagnosed in 1994. Research supports this connection, as moderate brain injuries increase Alzheimer’s risk 2.3 times, while severe injuries raise it 4.5 times.
Reagan’s presidency transformed America – ending the Cold War, spurring economic growth, and restoring national optimism. His personal experience with brain injury adds poignant context to his earlier advocacy, creating a legacy for millions affected by neurological conditions.