Martin Luther King Jr. never spoke directly about disability or brain injury, yet his civil rights movement built a legal foundation that protects millions of brain injury survivors today.
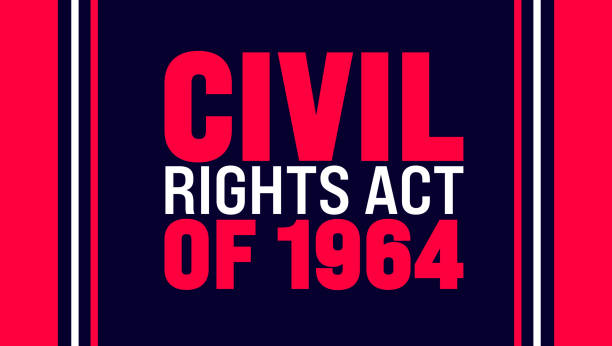
The connection lives in the law itself. Title VI of the Civil Rights Act (1964) declares that no person shall “be excluded from participation in, be denied the benefits of, or be subjected to discrimination” based on race. Section 504 of the Rehabilitation Act of 1973 and the Americans with Disabilities Act of 1990 both borrow this exact language, extending protections to people with disabilities, including brain injury survivors.
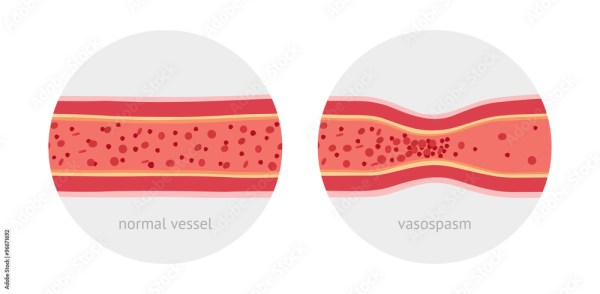
Tragically, the King family later experienced brain injury firsthand. On August 16, 2005, Coretta Scott King (1927-2006) suffered a stroke, leaving her paralyzed and unable to speak. Though she could never publicly address her condition, her eldest daughter Yolanda King (1955-2007) transformed the family’s pain into purpose, becoming National Ambassador for the American Stroke Association’s “Power to End Stroke” campaign. In her final speech in May 2007, Yolanda declared: “Everyone has the responsibility and power to take control of their health.”

King’s principle that “injustice anywhere is a threat to justice everywhere” applies to and protects brain injury survivors. Though he never marched for disability rights, his dream has expanded to embrace them.