The brain maintains executive function over the entire body. As we have all learned, when someone has the flu, it’s really the brain that “tells” them that their stomach hurts. However, what happens when the brain and its functioning therein are injured?
The medical field has been studying this for some time. About a decade ago, for example, the NIH concluded that a traumatic brain injury brings an increase in intestinal permeability.* (Beyond TBI, increased intestinal permeability can be cause by such things as excess alcohol consumption.) “Intestinal permeability is a barrier feature closely linked to the intestinal commensal microbiota as well as to the elements of the mucosal immune system.” The term is often used synonymously with “intestinal barrier,” even though the two do not have the same exact definition.
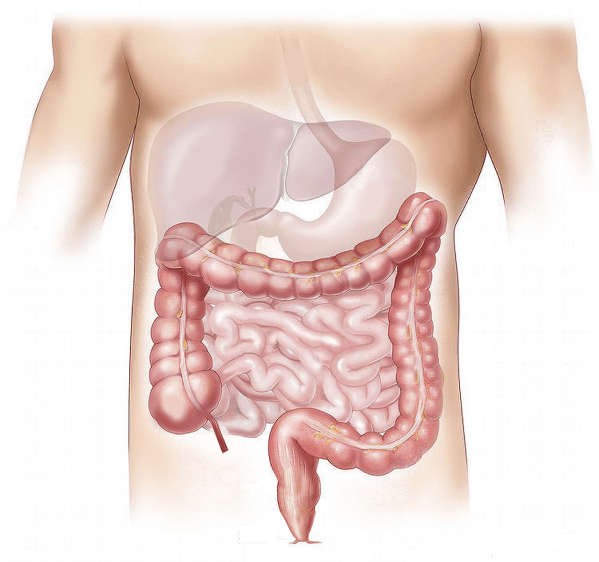
In 2015, the NIH found, “Deficits in intestinal permeability may underpin the chronic low-grade inflammation observed in disorders such as depression.” Depression is, of course, all too common among those with brain injury, so discovering one of the causes and perhaps finding a cure could be of extreme benefit. Last year, the University of Maryland again studied the correlation between traumatic brain injury and intestinal damage. (This study only examined the effects in mice.) To summarize their findings into one sentence, scientists now recognize that, “brain trauma can make the colon more permeable, potentially allowing harmful microbes to migrate from the intestine to other areas of the body, causing infection.” In essence, they found it to be a two-way street: the brain can “harm” the gastro system and the intestinal system can do the same to the brain. (At the moment, damage discovery seems to be the only goal. Perhaps fixing the problem and preventing later brain damage will come next.)
* As interesting as the above results are, traumatic brain injury is so named because it is severe and the resulting health problems likely go beyond the brain. Other internal and external organs may be affected by the incident. If the gastrointestinal system is physically harmed, it will no longer function in an optimal manner. Digestion may no longer be such an easy/painfree activity. Absorption of all nutrients may no longer be possible.